Your Complete Guide: Pregnancy Diet Chart Month by Month
Your Complete Guide: Pregnancy Diet Chart Month by Month
1.Introduction:
Welcome to Your Comprehensive Guide: Pregnancy Diet Chart Month by Month. Congratulations on your pregnancy journey! As you embark on this miraculous time, it’s essential to prioritize your health and nutrition for both you and your growing baby. In this guide, we will delve into every aspect of pregnancy nutrition, providing you with detailed month-by-month dietary recommendations to ensure a healthy and fulfilling pregnancy experience.
1: Understanding Pregnancy Nutrition
Before we delve into the specifics of each trimester’s dietary needs, it’s crucial to understand the foundational importance of nutrition during pregnancy. In this chapter, we will explore why nutrition matters, the key nutrients essential for a healthy pregnancy, and how your dietary choices can impact your baby’s development.
1.1 The Importance of Nutrition During Pregnancy: During pregnancy, your body undergoes significant changes to support the growth and development of your baby. Proper nutrition plays a fundamental role in ensuring these changes occur optimally. Here’s why nutrition is crucial during this period:
- Fueling Growth: Your baby’s development relies heavily on the nutrients you consume. Adequate nutrition provides the building blocks necessary for cell growth, organ development, and overall health.
- Supporting Maternal Health: Pregnancy places increased demands on your body, including higher energy requirements, changes in hormone levels, and adjustments to metabolism. A balanced diet helps support maternal health, reducing the risk of complications such as gestational diabetes, preeclampsia, and preterm birth.
- Enhancing Fetal Development: The nutrients you consume during pregnancy directly influence your baby’s growth and development. From neural tube formation to bone development, each stage of fetal growth requires specific nutrients to progress effectively.
- Promoting Long-Term Health: Research suggests that maternal nutrition during pregnancy can have lasting effects on the health and well-being of both mother and child. Optimal nutrition may reduce the risk of chronic diseases later in life, such as obesity, diabetes, and cardiovascular conditions.
1.2 Key Nutrients for Pregnancy and Their Functions: To support the unique needs of pregnancy, certain nutrients play critical roles in maternal and fetal health. Understanding these key nutrients and their functions is essential for crafting a well-rounded pregnancy diet:
- Folic Acid: Vital for neural tube development and preventing neural tube defects such as spina bifida.
- Iron: Supports the production of red blood cells and prevents maternal anemia, ensuring adequate oxygen supply to the baby.
- Calcium: Essential for bone and teeth development in the fetus, as well as maintaining maternal bone health.
- Protein: Provides the building blocks for fetal growth and development, supporting the formation of tissues and organs.
- Omega-3 Fatty Acids: Promote brain and eye development in the baby and may reduce the risk of preterm birth.
- Vitamin D: Facilitates calcium absorption, crucial for bone health and immune function.
- Vitamin C: Supports collagen formation, wound healing, and iron absorption, essential for both mother and baby’s health.
1.3 How Pregnancy Nutrition Impacts Baby’s Development: The nutrients you consume during pregnancy play a direct role in shaping your baby’s growth and development. Here’s how pregnancy nutrition impacts various aspects of fetal development:
- Neural Tube Formation: Adequate intake of folic acid before and during early pregnancy is crucial for preventing neural tube defects, such as spina bifida and anencephaly.
- Organ Development: Nutrients like iron, calcium, and protein are essential for the formation and function of vital organs such as the heart, lungs, kidneys, and brain.
- Bone Health: Calcium, vitamin D, and other minerals support the development of strong bones and teeth in the fetus, laying the foundation for skeletal health.
- Brain Development: Omega-3 fatty acids, particularly DHA (docosahexaenoic acid), are critical for brain and nervous system development, contributing to cognitive function and visual acuity.
- Immune System Function: Nutrients like vitamin C, vitamin D, and zinc play key roles in supporting the baby’s developing immune system, helping to protect against infections and illnesses both in utero and after birth.
2: First Trimester (Months 1-3)
The first trimester of pregnancy is a period of profound changes and adjustments for both the mother and the developing baby. During these crucial months, establishing a healthy diet sets the stage for a successful pregnancy journey. In this chapter, we will explore the dietary essentials for the first trimester, coping strategies for morning sickness, the importance of folic acid, crafting a meal plan tailored to your needs, and foods to avoid to ensure a smooth and healthy start to your pregnancy.
2.1 Early Pregnancy Diet Essentials: As your body begins to adapt to the changes of pregnancy, nourishing yourself with the right foods becomes paramount. Here are some essential components of an early pregnancy diet:
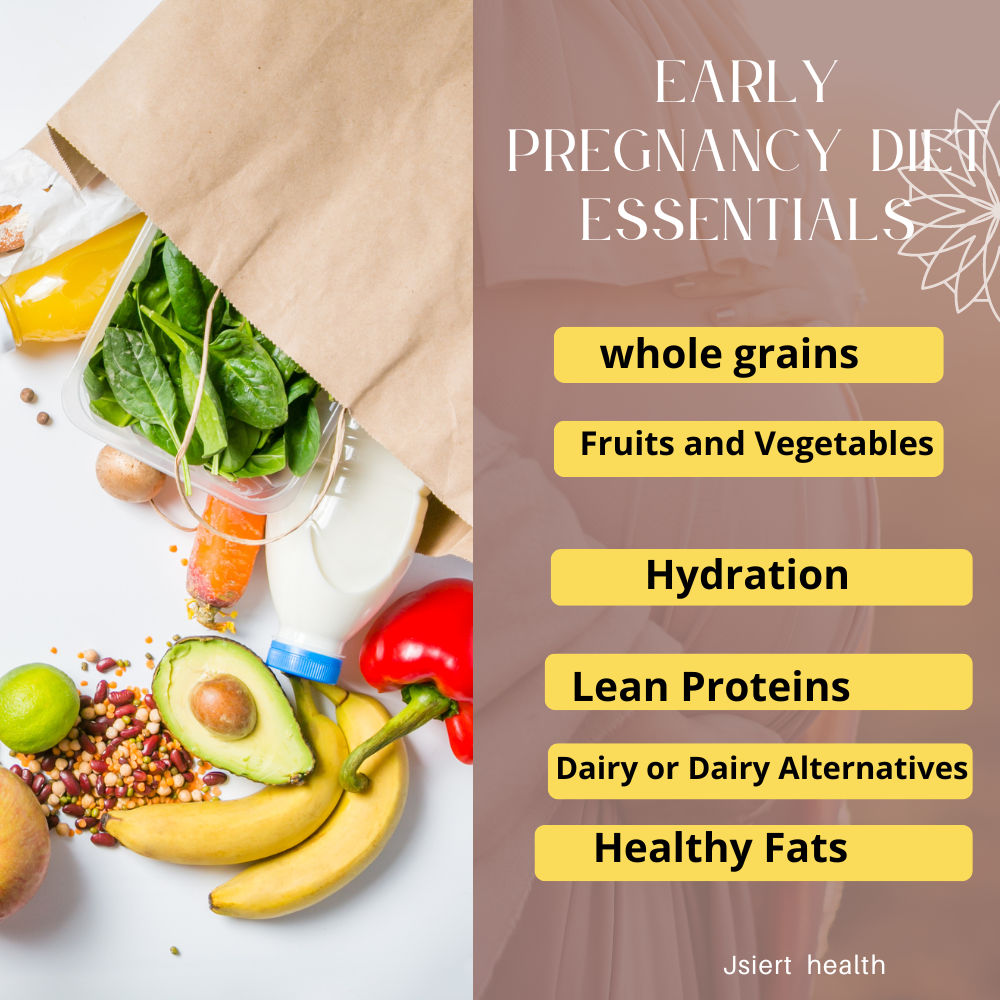
- Lean Proteins: Incorporate lean sources of protein such as poultry, fish, tofu, beans, and lentils to support fetal growth and development.
- Whole Grains: Choose whole grains like brown rice, quinoa, oats, and whole wheat bread to provide sustained energy and essential nutrients.
- Fruits and Vegetables: Load up on a variety of colorful fruits and vegetables rich in vitamins, minerals, and antioxidants to support overall health and immunity.
- Healthy Fats: Include sources of healthy fats such as avocados, nuts, seeds, and olive oil to support brain development and hormone production.
- Dairy or Dairy Alternatives: Ensure adequate intake of calcium and vitamin D by consuming dairy products or fortified alternatives like almond milk or soy milk.
- Hydration: Drink plenty of water throughout the day to stay hydrated and support the increased blood volume and fluid needs of pregnancy.
2.2 Coping with Morning Sickness: Foods to Ease Nausea: Morning sickness, a common symptom experienced during the first trimester, can make it challenging to maintain a healthy diet. Here are some foods and strategies to help ease nausea:
- Ginger: Incorporate ginger into your diet through ginger tea, ginger ale, or ginger candies, known for their anti-nausea properties.
- Small, Frequent Meals: Opt for smaller, more frequent meals and snacks to help manage nausea and prevent feelings of hunger.
- Bland Foods: Choose bland, easily digestible foods such as crackers, toast, rice, and bananas that are gentle on the stomach.
- Avoid Trigger Foods: Identify and avoid foods that trigger nausea, such as spicy or greasy foods, strong-smelling foods, and foods with strong flavors.
- Stay Hydrated: Sip on clear fluids like water, herbal teas, or electrolyte drinks to stay hydrated and prevent dehydration associated with vomiting.
2.3 Folic Acid and Its Role in Early Pregnancy: Folic acid, a B-vitamin essential for fetal development, plays a crucial role in preventing neural tube defects. Here’s why folic acid is important during early pregnancy:
- Neural Tube Development: Folic acid is necessary for the formation of the neural tube, which develops into the baby’s brain and spinal cord.
- Prevention of Birth Defects: Adequate folic acid intake before and during early pregnancy can significantly reduce the risk of neural tube defects such as spina bifida and anencephaly.
- Recommended Intake: Pregnant women are advised to take a daily prenatal vitamin containing 400-800 micrograms of folic acid, in addition to consuming folate-rich foods such as leafy greens, citrus fruits, beans, and fortified grains.
2.4 Crafting Your First Trimester Meal Plan: Creating a well-balanced meal plan tailored to your needs is essential for meeting your nutritional requirements during the first trimester. Here’s how to craft a nutritious meal plan:
- Start with a Foundation: Build your meals around a variety of nutrient-dense foods, including lean proteins, whole grains, fruits, and vegetables.
- Include Folate-Rich Foods: Ensure adequate intake of folic acid by incorporating folate-rich foods such as leafy greens, legumes, citrus fruits, and fortified grains into your meals.
- Address Specific Cravings and Aversions: Listen to your body’s cravings and aversions, but aim to make healthy choices that satisfy your nutritional needs.
- Plan for Snacks: Have healthy snacks on hand to curb hunger between meals and provide sustained energy throughout the day.
- Stay Flexible: Be flexible with your meal plan and make adjustments as needed to accommodate changes in appetite, cravings, and food tolerances.
2.5 Foods to Avoid During the First Trimester: While many foods are safe to consume during pregnancy, some should be avoided or limited due to potential risks to the baby’s health. Here are some foods to avoid during the first trimester:
- Raw or Undercooked Meats: To reduce the risk of foodborne illness, avoid consuming raw or undercooked meats, poultry, seafood, and eggs.
- Unpasteurized Dairy Products: Steer clear of unpasteurized milk, cheeses, and dairy products, which may contain harmful bacteria such as listeria.
- High-Mercury Fish: Limit consumption of high-mercury fish such as swordfish, shark, king mackerel, and tilefish, as they may harm the baby’s developing nervous system.
- Deli Meats and Processed Foods: Minimize intake of deli meats, hot dogs, and processed foods that may be contaminated with listeria bacteria.
- Caffeine and Alcohol: Limit caffeine intake to no more than 200 milligrams per day and avoid alcohol altogether during pregnancy to reduce the risk of birth defects and developmental issues.
Conclusion: The first trimester of pregnancy is a critical time for establishing healthy dietary habits that will support both maternal and fetal health throughout the pregnancy journey. By focusing on early pregnancy diet essentials, coping strategies for morning sickness, the importance of folic acid, crafting a meal plan, and avoiding potentially harmful foods, you can lay the groundwork for a successful and nourishing pregnancy experience. In the following chapters, we will continue to explore dietary recommendations for the second and third trimesters, providing you with the knowledge and tools to navigate each stage of pregnancy with confidence and ease.
3: Second Trimester (Months 4-6)
As you enter the second trimester of your pregnancy journey, your body and your baby continue to undergo significant changes. During these months, it’s crucial to adjust your diet to meet the evolving needs of both you and your growing baby. In this chapter, we will explore the specific nutrient requirements for the second trimester, focusing on calcium-rich foods for bone development, strategies for managing gestational diabetes through diet, tips for maintaining energy levels with smart snacking, and providing sample meal plans tailored to this stage of pregnancy.
3.1 Nutrient Needs in the Second Trimester: The second trimester brings about unique nutritional requirements to support the continued growth and development of your baby. Here’s a closer look at the key nutrients needed during this stage:
- Protein: Essential for the growth and repair of tissues, protein needs increase during the second trimester to support the developing baby’s rapid growth.
- Calcium: Crucial for bone and teeth development in the fetus, calcium requirements rise during the second trimester to meet the demands of skeletal growth.
- Iron: Iron needs remain elevated during the second trimester to support the increased blood volume and oxygen transport to the baby.
- Vitamin D: Necessary for calcium absorption and bone health, adequate vitamin D intake is essential during the second trimester.
- Omega-3 Fatty Acids: Important for brain and eye development in the baby, omega-3 fatty acids play a vital role during the second trimester.
3.2 Building Strong Bones: Calcium-Rich Foods for Pregnancy: During the second trimester, calcium becomes particularly important for the development of your baby’s bones and teeth. Here are some calcium-rich foods to incorporate into your diet:
- Dairy Products: Milk, cheese, yogurt, and kefir are excellent sources of calcium, providing essential nutrients for bone health.
- Leafy Greens: Include leafy greens such as kale, spinach, collard greens, and bok choy in your meals to boost your calcium intake.
- Fortified Foods: Opt for fortified foods like fortified orange juice, tofu, and breakfast cereals to increase your calcium consumption.
- Nuts and Seeds: Almonds, sesame seeds, and chia seeds are nutritious snacks that contain calcium and other essential nutrients.
- Fish: Choose fish with edible bones such as canned salmon and sardines to add calcium to your diet.
3.3 Managing Gestational Diabetes Through Diet: Gestational diabetes, a condition characterized by high blood sugar levels during pregnancy, requires careful management through diet and lifestyle changes. Here are some dietary strategies to help manage gestational diabetes:
- Monitor Carbohydrate Intake: Pay attention to your carbohydrate intake and choose complex carbohydrates that are high in fiber and low in added sugars.
- Focus on Balanced Meals: Aim for balanced meals that include a combination of lean protein, healthy fats, and complex carbohydrates to help stabilize blood sugar levels.
- Portion Control: Practice portion control to avoid large spikes in blood sugar levels after meals.
- Regular Meal Times: Stick to regular meal times and avoid skipping meals to help regulate blood sugar levels throughout the day.
- Stay Active: Incorporate regular physical activity into your routine to improve insulin sensitivity and help control blood sugar levels.
3.4 Maintaining Energy Levels with Smart Snacking: As your energy needs increase during the second trimester, smart snacking can help keep you fueled and satisfied between meals. Here are some tips for maintaining energy levels with smart snacking:
- Choose Nutrient-Dense Foods: Opt for snacks that are rich in nutrients such as fruits, vegetables, nuts, seeds, and whole grains.
- Pair Protein with Carbohydrates: Pairing protein with carbohydrates can help provide sustained energy and prevent blood sugar fluctuations.
- Plan Ahead: Plan and prepare healthy snacks in advance to have on hand when hunger strikes.
- Hydrate: Stay hydrated by drinking plenty of water throughout the day, as dehydration can contribute to fatigue.
- Listen to Your Body: Pay attention to your hunger and fullness cues, and eat when you’re hungry to maintain energy levels and support your baby’s growth.
3.5 Sample Meal Plans for the Second Trimester: Here are two sample meal plans to help you meet your nutritional needs during the second trimester:
Meal Plan 1:
- Breakfast: Greek yogurt with berries and granola
- Snack: Apple slices with almond butter
- Lunch: Quinoa salad with mixed vegetables and grilled chicken
- Snack: Carrot sticks with hummus
- Dinner: Baked salmon with roasted sweet potatoes and steamed broccoli
Meal Plan 2:
- Breakfast: Whole grain toast with avocado and scrambled eggs
- Snack: Greek yogurt with sliced almonds and honey
- Lunch: Lentil soup with a side salad and whole grain roll
- Snack: Cottage cheese with pineapple chunks
- Dinner: Stir-fried tofu with mixed vegetables and brown rice
Conclusion: As you navigate through the second trimester of your pregnancy, focusing on nutrient-dense foods, managing gestational diabetes through diet, and maintaining energy levels with smart snacking are essential for supporting your health and the health of your baby. By incorporating calcium-rich foods, implementing strategies for managing gestational diabetes, and following sample meal plans tailored to this stage of pregnancy, you can ensure that you’re meeting your nutritional needs and enjoying a healthy and fulfilling pregnancy experience. In the following chapter, we will continue to explore dietary recommendations for the third trimester, providing you with the knowledge and tools to thrive throughout the remainder of your pregnancy journey.
4: Third Trimester (Months 7-9)

As you enter the final stretch of your pregnancy journey, the third trimester brings about its own set of nutritional considerations and challenges. During these months, it’s essential to focus on meeting increased caloric needs, maintaining adequate iron levels to prevent anemia, managing common discomforts like heartburn, preparing your body for labor with nutrient-dense foods, and staying hydrated for both you and your baby’s well-being. In this chapter, we will explore these topics in detail to help you navigate the final months of your pregnancy with confidence and ease.
4.1 Meeting Increased Caloric Needs in the Third Trimester: As your baby continues to grow rapidly during the third trimester, your caloric needs increase to support both fetal development and your body’s changing needs. Here’s how to ensure you’re meeting your increased caloric needs:
- Listen to Your Body: Pay attention to hunger cues and eat when you’re hungry to ensure you’re consuming enough calories to support your energy levels and your baby’s growth.
- Choose Nutrient-Dense Foods: Focus on nutrient-dense foods that provide essential vitamins, minerals, and macronutrients without excess calories, such as fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Eat Regular Meals and Snacks: Aim for three balanced meals and 1-2 snacks per day to help maintain stable blood sugar levels and prevent excessive hunger.
- Avoid Empty Calories: Minimize consumption of sugary snacks, processed foods, and beverages high in added sugars, as they provide little nutritional value and can contribute to excessive weight gain.
4.2 Iron-Rich Foods to Prevent Anemia: Iron deficiency anemia is common during pregnancy and can lead to fatigue, weakness, and other complications. To prevent anemia and support maternal and fetal health during the third trimester, focus on incorporating iron-rich foods into your diet:
- Lean Meats: Include lean sources of meat such as beef, pork, and poultry in your meals to boost your iron intake.
- Leafy Greens: Incorporate leafy greens like spinach, kale, and Swiss chard into salads, soups, and stir-fries to increase your iron consumption.
- Legumes: Beans, lentils, and chickpeas are excellent plant-based sources of iron that can be added to salads, stews, and wraps.
- Fortified Grains: Choose fortified cereals, bread, pasta, and rice to boost your iron intake, especially if you follow a vegetarian or vegan diet.
- Vitamin C-Rich Foods: Pair iron-rich foods with sources of vitamin C such as citrus fruits, bell peppers, and strawberries to enhance iron absorption.
4.3 Dealing with Heartburn: Foods to Soothe Discomfort: Heartburn, a common discomfort during the third trimester, can be exacerbated by hormonal changes and the growing uterus putting pressure on the stomach. Here are some foods and strategies to help soothe heartburn:
- Eat Smaller, More Frequent Meals: Opt for smaller meals and snacks throughout the day to prevent overfilling your stomach and minimize acid reflux.
- Choose Low-Acid Foods: Select foods that are lower in acidity, such as bananas, oatmeal, yogurt, and lean proteins, to reduce the likelihood of triggering heartburn.
- Avoid Trigger Foods: Identify and avoid foods that tend to trigger heartburn, such as spicy foods, citrus fruits, tomatoes, and chocolate.
- Stay Upright After Eating: Avoid lying down immediately after eating to allow gravity to help keep stomach acids from refluxing into the esophagus.
- Use Pillows for Elevation: Prop yourself up with pillows while sleeping to keep your upper body elevated and reduce nighttime heartburn.
4.4 Preparing for Labor with Nutrient-Dense Foods: As you approach the end of your pregnancy, focusing on nutrient-dense foods can help prepare your body for labor and delivery. Here are some foods to include in your diet to support the birthing process:
- Healthy Fats: Incorporate sources of healthy fats such as avocados, nuts, seeds, and olive oil to provide sustained energy and support hormone production.
- Lean Proteins: Choose lean sources of protein such as poultry, fish, tofu, and beans to promote muscle strength and endurance during labor.
- Complex Carbohydrates: Opt for complex carbohydrates like whole grains, fruits, and vegetables to provide long-lasting energy and stabilize blood sugar levels.
- Hydrating Foods: Consume hydrating foods such as watermelon, cucumbers, and oranges to maintain hydration levels and support uterine contractions.
4.5 Tips for Hydration and Water Intake in the Third Trimester: Staying hydrated is crucial during the third trimester to support your body’s increased fluid needs and maintain optimal health for you and your baby. Here are some tips for staying hydrated and meeting your water intake goals:
- Drink Plenty of Water: Aim to drink at least 8-10 cups of water per day, or more if you’re physically active or experiencing hot weather.
- Infuse Water with Flavor: Add natural flavor to your water by infusing it with fresh fruits, herbs, or cucumber slices for a refreshing twist.
- Consume Hydrating Foods: Incorporate hydrating foods such as soups, smoothies, fruits, and vegetables into your meals and snacks to increase your fluid intake.
- Carry a Water Bottle: Keep a reusable water bottle with you throughout the day to remind yourself to stay hydrated and make it easy to sip on water wherever you go.
- Monitor Urine Color: Check the color of your urine regularly; pale yellow or clear urine indicates adequate hydration, while dark yellow or amber urine may signal dehydration.
Conclusion: As you navigate through the third trimester of your pregnancy journey, focusing on meeting increased caloric needs, maintaining adequate iron levels, managing heartburn discomfort, preparing your body for labor with nutrient-dense foods, and staying hydrated are essential for your health and the health of your baby. By incorporating nutrient-rich foods, implementing strategies for managing common discomforts, and prioritizing hydration, you can support your body’s needs and prepare for the final stages of pregnancy and childbirth with confidence and ease. In the following chapter, we will conclude our exploration of pregnancy nutrition, providing you with additional resources and guidance for postpartum health and wellness.
5: Postpartum Nutrition
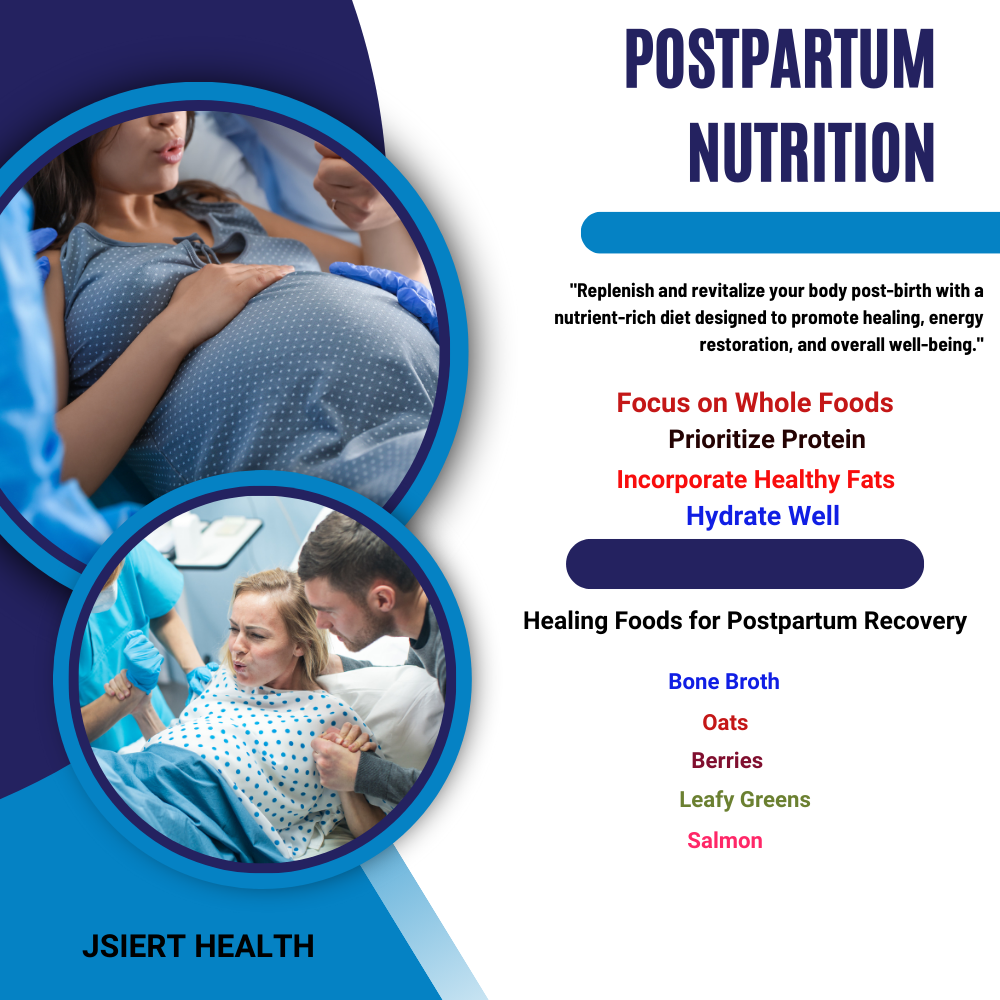
Congratulations on the arrival of your precious little one! As you transition into the postpartum period, it’s crucial to prioritize your nutrition to support your recovery, energy levels, and overall well-being. In this chapter, we will delve into the importance of nourishing your body after birth, explore healing foods for postpartum recovery, discuss the breastfeeding diet to support milk production, offer guidance on balancing weight loss goals with nutritional needs, and provide practical meal prep ideas for busy new moms. Let’s dive into these topics to ensure you feel nourished and supported during this special time.
5.1 Nourishing Your Body After Birth: The postpartum period is a time of immense change and adjustment for your body. Nourishing yourself with wholesome, nutrient-rich foods is essential for supporting your recovery and replenishing vital nutrients. Here’s how to nourish your body after birth:
- Focus on Whole Foods: Choose whole, unprocessed foods such as fruits, vegetables, lean proteins, whole grains, and healthy fats to provide essential nutrients and support your overall health.
- Prioritize Protein: Include sources of lean protein like chicken, fish, tofu, beans, and eggs in your meals to aid in tissue repair and muscle recovery.
- Incorporate Healthy Fats: Include sources of healthy fats such as avocados, nuts, seeds, and olive oil to support hormone regulation and brain function.
- Hydrate Well: Drink plenty of water throughout the day to stay hydrated and support milk production if breastfeeding.
5.2 Healing Foods for Postpartum Recovery: Certain foods can aid in your postpartum recovery by providing essential nutrients and supporting your body’s healing process. Here are some healing foods to incorporate into your diet:
- Bone Broth: Rich in collagen and minerals, bone broth can support gut health, aid in digestion, and promote tissue repair.
- Oats: Oats are a great source of fiber, which can help regulate digestion and stabilize blood sugar levels. They also contain compounds that may support milk production if breastfeeding.
- Berries: Berries are packed with antioxidants and vitamins that can support immune function and aid in tissue repair.
- Leafy Greens: Greens like spinach, kale, and Swiss chard are rich in vitamins, minerals, and antioxidants that support overall health and recovery.
- Salmon: Salmon is an excellent source of omega-3 fatty acids, which have anti-inflammatory properties and may support postpartum mood and recovery.
5.3 Breastfeeding Diet: Supporting Milk Production: If you’re breastfeeding, your nutritional needs are elevated to support milk production and meet your own energy requirements. Here are some tips for maintaining a breastfeeding-friendly diet:

- Stay Hydrated: Drink plenty of water throughout the day to support hydration and milk production.
- Eat Regular Meals and Snacks: Aim for balanced meals and snacks throughout the day to provide sustained energy and nutrients for both you and your baby.
- Include Galactagogues: Certain foods like oats, fenugreek, and brewer’s yeast are believed to support milk production. Incorporate these into your diet as needed.
- Consume Adequate Calories: Breastfeeding requires extra energy, so be sure to eat enough calories to support milk production and your own nutritional needs.
5.4 Balancing Weight Loss Goals with Nutritional Needs: Many new moms are eager to regain their pre-pregnancy weight after giving birth, but it’s essential to balance weight loss goals with your body’s nutritional needs, especially if you’re breastfeeding. Here are some tips for finding that balance:
- Focus on Nutrient-Dense Foods: Choose foods that are rich in nutrients and low in empty calories to ensure you’re meeting your nutritional needs while still supporting weight loss goals.
- Practice Portion Control: Pay attention to portion sizes and listen to your body’s hunger and fullness cues to avoid overeating.
- Be Patient: Remember that weight loss takes time, especially during the postpartum period. Aim for gradual, sustainable weight loss rather than rapid changes.
- Prioritize Self-Care: Focus on nourishing your body with wholesome foods, staying active in a way that feels good for you, and getting plenty of rest and relaxation.
5.5 Meal Prep Ideas for Busy New Moms: As a new mom, finding time to prepare nutritious meals can be challenging. Meal prep can help streamline the process and ensure you have nourishing options on hand when you need them. Here are some meal prep ideas for busy new moms:
- Prep Ingredients in Advance: Wash, chop, and portion out fruits, vegetables, and other ingredients at the beginning of the week to make meal preparation easier.
- Cook in Batches: Prepare large batches of soups, stews, casseroles, or grains that can be portioned out and stored for quick and easy meals throughout the week.
- Freeze Extras: Freeze individual portions of meals or meal components for future use when you’re short on time or energy.
- Keep Snacks Handy: Prepare healthy snacks like cut-up vegetables, fruit, nuts, yogurt, or energy balls to have on hand for quick and convenient snacking.
Conclusion: As you navigate the postpartum period and adjust to life as a new mom, prioritizing your nutrition is key to supporting your recovery, energy levels, and overall well-being. By nourishing your body with healing foods, supporting milk production through a breastfeeding-friendly diet, balancing weight loss goals with nutritional needs, and embracing practical meal prep strategies, you can ensure you feel nourished and supported during this special time. Remember to listen to your body, be patient with yourself, and seek support when needed as you embark on this incredible journey of motherhood. Wishing you health, happiness, and abundant nourishment in the postpartum period and beyond!
6: Overcoming Common Challenges
Throughout pregnancy, many women encounter various challenges related to nutrition and dietary habits. In this chapter, we will address some of the most common hurdles faced by expectant mothers and provide practical strategies for overcoming them. From managing food aversions and cravings to addressing concerns about weight gain, making healthy food choices on a budget, dealing with dietary restrictions, and knowing when to seek professional guidance, we’ll explore effective approaches to ensure optimal nutrition and well-being during pregnancy.
6.1 Managing Food Aversions and Cravings: Food aversions and cravings are common during pregnancy and can sometimes make it challenging to maintain a balanced diet. Here’s how to manage them effectively:
- Listen to Your Body: Pay attention to your body’s cues and honor your cravings within reason, while also ensuring you’re meeting your nutritional needs.
- Find Alternatives: If you have aversions to certain foods, try substituting them with similar alternatives that provide similar nutrients.
- Opt for Nutrient-Dense Options: When experiencing cravings, choose nutrient-dense options whenever possible to satisfy cravings while nourishing your body.
- Practice Moderation: Indulge in cravings occasionally but aim for balance and moderation to avoid excessive intake of unhealthy foods.
- Experiment with Preparation Methods: If certain foods trigger aversions, try experimenting with different preparation methods to make them more palatable.
6.2 Addressing Concerns About Weight Gain: Weight gain is a natural part of pregnancy, but many women have concerns about gaining too much or too little weight. Here’s how to address concerns about weight gain:
- Focus on Health, Not Numbers: Instead of fixating on the number on the scale, focus on eating a balanced diet, staying active, and listening to your body’s hunger and fullness cues.
- Trust Your Healthcare Provider: Work with your healthcare provider to establish appropriate weight gain goals based on your pre-pregnancy weight, BMI, and overall health.
- Monitor Weight Gain Trends: Rather than obsessing over daily fluctuations, focus on trends in weight gain over time to ensure you’re on track.
- Embrace Body Positivity: Remember that weight gain is a natural and necessary part of pregnancy and focus on appreciating your body’s incredible ability to nurture and support new life.
6.3 Making Healthy Food Choices on a Budget: Eating healthily during pregnancy doesn’t have to break the bank. Here are some tips for making healthy food choices on a budget:
- Plan Ahead: Create a weekly meal plan and grocery list to avoid impulse purchases and ensure you have everything you need for nutritious meals.
- Buy in Bulk: Purchase staple items like grains, beans, and frozen fruits and vegetables in bulk to save money and reduce waste.
- Choose Seasonal Produce: Opt for fruits and vegetables that are in season, as they tend to be more affordable and flavorful.
- Shop Sales and Discounts: Take advantage of sales, coupons, and discounts to save money on groceries without compromising on nutrition.
- Cook at Home: Prepare meals at home whenever possible, as eating out tends to be more expensive and less nutritious.
6.4 Dealing with Dietary Restrictions During Pregnancy: If you have dietary restrictions or follow a special diet, it’s essential to ensure you’re still meeting your nutritional needs during pregnancy. Here’s how to navigate dietary restrictions:
- Work with a Healthcare Provider: Consult with your healthcare provider or a registered dietitian to develop a meal plan that accommodates your dietary restrictions while meeting your nutritional needs.
- Focus on Alternative Sources: Identify alternative sources of nutrients that may be restricted in your diet and incorporate them into your meals and snacks.
- Consider Supplementation: In some cases, supplementation may be necessary to ensure you’re getting adequate nutrients that are lacking in your diet due to restrictions.
- Stay Informed: Educate yourself about your dietary restrictions and learn how to read food labels to identify potential allergens or ingredients to avoid.
- Connect with Support Groups: Seek out support groups or online communities of individuals who share similar dietary restrictions for tips, advice, and encouragement.
6.5 Seeking Professional Guidance: When to Consult a Nutritionist or Dietitian: If you’re unsure about your nutritional needs during pregnancy or struggling to meet them, it may be beneficial to seek professional guidance from a nutritionist or dietitian. Here are some signs that indicate it’s time to consult a professional:
- Difficulty meeting nutritional needs due to dietary restrictions, aversions, or other challenges.
- Concerns about weight gain or loss that are impacting your health or well-being.
- Complications such as gestational diabetes, hypertension, or other medical conditions that require dietary management.
- Need for personalized guidance and support in developing a meal plan tailored to your individual needs and preferences.
- Desire for evidence-based information and strategies to optimize nutrition and promote a healthy pregnancy.
Conclusion: Overcoming common challenges related to nutrition during pregnancy requires a combination of practical strategies, self-awareness, and sometimes professional guidance. By managing food aversions and cravings, addressing concerns about weight gain, making healthy food choices on a budget, navigating dietary restrictions, and knowing when to seek professional help, you can ensure that you and your baby receive the nutrients needed for a healthy pregnancy and beyond. In the final chapter, we will recap key takeaways and provide additional resources to support you on your journey to optimal nutrition and wellness during pregnancy.
7: Conclusion
Congratulations! You’ve embarked on an incredible journey through pregnancy, filled with moments of joy, anticipation, and perhaps a few challenges along the way. As you near the end of this transformative experience, it’s essential to reflect on the knowledge and nutrition strategies you’ve gained to support yourself and your growing baby. In this final chapter, we’ll recap key takeaways from your pregnancy nutrition journey, discuss the importance of empowering yourself through knowledge and nutrition, celebrate the unique milestones of your pregnancy, and provide additional resources to support you as you transition into motherhood.
7.1 Recap of Key Takeaways: Throughout this guide, you’ve learned valuable insights and practical strategies for optimizing your nutrition during pregnancy. Let’s recap some of the key takeaways:
- Understanding the importance of nutrition during pregnancy and the role it plays in supporting your health and the development of your baby.
- Identifying key nutrients needed during each trimester and incorporating them into a balanced diet.
- Managing common challenges such as food aversions, cravings, weight gain concerns, and dietary restrictions with confidence and practical strategies.
- Navigating the unique nutritional needs of postpartum recovery and breastfeeding.
- Knowing when to seek professional guidance from healthcare providers, nutritionists, or dietitians for personalized support.
7.2 Empowering Yourself Through Knowledge and Nutrition: Empowering yourself with knowledge and nutrition is essential for a healthy and fulfilling pregnancy journey. By understanding the importance of nourishing your body with nutrient-dense foods, making informed choices, and seeking support when needed, you can take control of your health and well-being during this transformative time.
- Stay Informed: Continue to educate yourself about pregnancy nutrition, postpartum recovery, and breastfeeding to make informed decisions that support your health and the health of your baby.
- Trust Your Instincts: Listen to your body’s cues and trust your instincts when it comes to making choices about food, exercise, and self-care during pregnancy and beyond.
- Advocate for Yourself: Be an advocate for your own health by communicating openly with your healthcare providers, asking questions, and seeking second opinions if needed.
- Practice Self-Compassion: Remember to be kind to yourself and practice self-compassion as you navigate the ups and downs of pregnancy and motherhood. Celebrate your accomplishments and give yourself grace during challenging times.
7.3 Celebrating Your Pregnancy Journey: As you approach the end of your pregnancy journey, take a moment to celebrate the incredible milestone you’ve reached. Whether you’ve experienced moments of excitement, anticipation, or uncertainty, each step has been a part of your unique and beautiful journey to motherhood.
- Reflect on Milestones: Take time to reflect on the milestones you’ve achieved throughout your pregnancy, from the first flutter of movement to the final weeks of anticipation.
- Capture Memories: Capture memories of your pregnancy journey through photos, journaling, or creating a scrapbook to cherish for years to come.
- Share Your Story: Share your pregnancy story with loved ones, friends, or online communities to celebrate your journey and offer support and encouragement to others.
- Pamper Yourself: Treat yourself to a special celebration or self-care ritual to honor the incredible journey your body has undertaken over the past nine months.
7.4 Additional Resources for Continued Support: As you prepare to welcome your baby and embark on the adventure of motherhood, remember that support is available every step of the way. Here are some additional resources to support you on your journey:
- Online Communities: Join online forums or social media groups for expectant mothers and new moms to connect with others who are experiencing similar joys and challenges.
- Books and Websites: Explore reputable books, websites, and blogs dedicated to pregnancy, childbirth, and parenting for evidence-based information and advice.
- Healthcare Providers: Lean on your healthcare providers, including obstetricians, midwives, lactation consultants, and pediatricians, for guidance and support throughout your pregnancy and beyond.
- Support Groups: Seek out local support groups or breastfeeding circles for additional support, encouragement, and camaraderie with other new moms in your community.
- Postpartum Services: Consider enrolling in postpartum support services such as lactation classes, infant care workshops, or postpartum doula support to ease the transition into motherhood.
Frequently Asked Questions (FAQ) for Your Complete Guide: Pregnancy Diet Chart Month by Month
- Why is nutrition important during pregnancy?
- Nutrition plays a vital role in supporting the health and development of both the mother and the baby during pregnancy. Adequate intake of essential nutrients is crucial for fetal growth, maternal health, and overall well-being.
- What are the key nutrients needed during pregnancy?
- Throughout pregnancy, several key nutrients are essential for optimal health. These include folic acid, iron, calcium, omega-3 fatty acids, vitamin D, and protein, among others. Each trimester may have specific nutrient requirements that are important for the baby’s growth and development.
- How can I create a balanced diet during pregnancy?
- A balanced diet during pregnancy should include a variety of nutrient-dense foods from all food groups. Focus on incorporating fruits, vegetables, whole grains, lean proteins, and healthy fats into your meals. It’s also essential to stay hydrated by drinking plenty of water throughout the day.
- What foods should I avoid during pregnancy?
- Certain foods should be avoided or limited during pregnancy to minimize the risk of foodborne illness or harm to the baby. These may include unpasteurized dairy products, raw or undercooked meats and seafood, deli meats, high-mercury fish, and excessive caffeine or alcohol.
- How can I cope with morning sickness and food aversions?
- Morning sickness and food aversions are common during the first trimester of pregnancy. To cope with these symptoms, try eating small, frequent meals throughout the day, avoiding strong odors or triggers, staying hydrated, and consuming bland, easy-to-digest foods like crackers or ginger tea.
- Is it safe to lose weight during pregnancy?
- While weight gain is expected during pregnancy, some women may need to manage their weight due to pre-existing conditions or medical recommendations. It’s essential to consult with your healthcare provider before attempting to lose weight during pregnancy to ensure it’s done safely and without compromising the baby’s health.
- What are some healthy snack options for pregnant women?
- Healthy snacks for pregnant women include fruits, vegetables with hummus or yogurt dip, nuts and seeds, whole-grain crackers with cheese, Greek yogurt, smoothies, and homemade energy bars. These snacks provide essential nutrients and can help curb hunger between meals.
- How can I ensure I’m getting enough nutrients during each trimester?
- To ensure you’re getting enough nutrients during each trimester, focus on consuming a balanced diet that includes a variety of nutrient-dense foods. Consider incorporating prenatal vitamins as recommended by your healthcare provider to fill any nutritional gaps.
- What are some tips for managing gestational diabetes through diet?
- Managing gestational diabetes through diet involves monitoring carbohydrate intake, choosing complex carbohydrates with a low glycemic index, spreading out carbohydrate intake throughout the day, and incorporating lean proteins and healthy fats into meals and snacks. Regular exercise and monitoring blood sugar levels are also important components of managing gestational diabetes.
- When should I consult a healthcare provider or nutritionist during pregnancy?
- It’s essential to consult with a healthcare provider or nutritionist if you have any concerns about your diet, weight gain, or overall health during pregnancy. Additionally, seek professional guidance if you have specific dietary restrictions, medical conditions, or need personalized recommendations for managing your nutrition during pregnancy.