How to Check for Uterine Fibroids at Home: Early Signs and Symptoms
Uterine Fibroids
1. Understanding Uterine Fibroids

Uterine fibroids, also known as leiomyomas or myomas, are benign tumors that arise from the smooth muscle tissue of the uterus. They can vary greatly in size, from microscopic to large masses that distort the uterus. Fibroids are categorized based on their location:
- Intramural Fibroids: Found within the muscular wall of the uterus.
- Submucosal Fibroids: Protrude into the uterine cavity, often causing heavy bleeding.
- Subserosal Fibroids: Extend from the outer surface of the uterus.
- Pedunculated Fibroids: Attached to the uterus by a thin stalk, which can sometimes twist and cause severe pain.
2. Early Signs and Symptoms
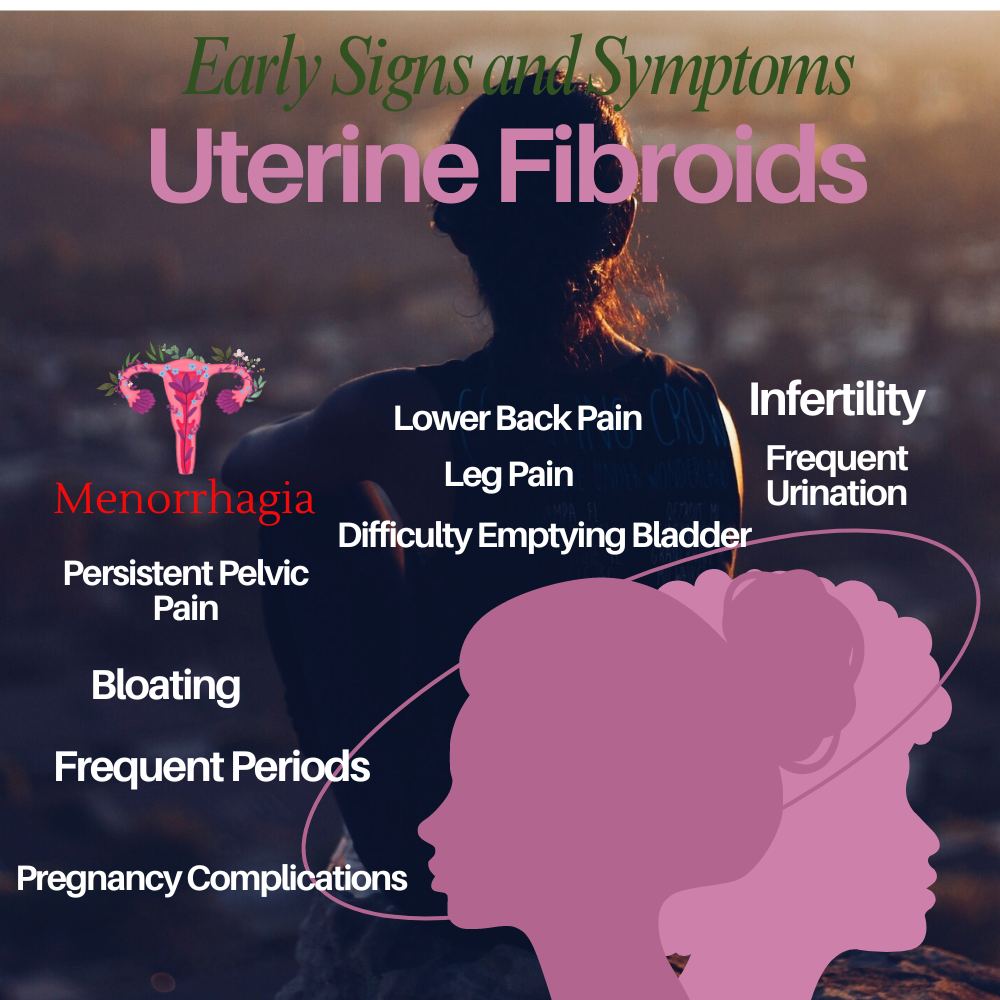
a. Heavy Menstrual Bleeding
- Menorrhagia: Significantly heavy and prolonged menstrual bleeding. Women may need to change sanitary protection frequently, often soaking through pads or tampons within an hour.
- Clots: The presence of large, dark red blood clots during menstruation.
b. Pelvic Pain and Pressure
- Persistent Pelvic Pain: Ongoing discomfort or pain in the pelvic region that is not related to the menstrual cycle.
- Pelvic Pressure: A sensation of fullness or pressure in the lower abdomen, which may feel similar to early pregnancy.
c. Abdominal Swelling
- Bloating: Persistent bloating that does not fluctuate with dietary changes or digestive processes.
- Visible Enlargement: Noticeable increase in abdominal size, resembling pregnancy, due to the size of the fibroids.
d. Menstrual Irregularities
- Frequent Periods: Menstrual cycles occurring more frequently than the typical 28-day interval.
- Prolonged Periods: Menstrual bleeding lasting longer than seven days.
e. Reproductive Issues
- Infertility: Difficulty in conceiving, as fibroids can distort the shape of the uterus or block the fallopian tubes.
- Pregnancy Complications: Increased risk of miscarriage, preterm birth, and need for cesarean delivery due to the presence of fibroids.
f. Urinary and Bowel Symptoms
- Frequent Urination: Increased need to urinate due to fibroids pressing on the bladder.
- Difficulty Emptying Bladder: Sensation of incomplete bladder emptying.
- Constipation: Chronic constipation or discomfort during bowel movements due to fibroids pressing on the rectum.
g. Back and Leg Pain
- Lower Back Pain: Persistent pain in the lower back, especially if fibroids press on spinal nerves.
- Leg Pain: Radiating pain down the legs caused by pressure on nerves.
3. Self-Assessment Tips
a. Track Menstrual Cycle
- Use a Period Tracker: Apps like Clue, Flo, or a physical calendar can help track the start and end dates of periods, flow intensity, and any unusual patterns.
- Note Blood Flow: Document the heaviness of bleeding, the presence of clots, and any other unusual characteristics.
b. Monitor Pelvic Pain
- Pain Diary: Keep a journal of any pelvic pain, noting its intensity, duration, and triggers or alleviating factors.
c. Observe Abdominal Changes
- Measure Waistline: Regularly measure and record your waistline at the same point to detect any abnormal growth or bloating.
- Check for Bloating: Pay attention to persistent bloating that is not related to diet or digestion.
d. Note Urinary and Bowel Changes
- Urination Frequency: Track how often you need to urinate and any difficulties, such as urgency or incomplete emptying.
- Bowel Movements: Record any changes in bowel habits, including frequency and difficulty of bowel movements.
e. Monitor Reproductive Health
- Track Fertility Signs: If trying to conceive, monitor ovulation signs and track any difficulties or irregularities.
- Document Pregnancy Symptoms: Note any unusual symptoms or complications during pregnancy and inform your healthcare provider.
4. When to Seek Medical Help
Persistent symptoms warrant professional evaluation. Medical assessment may include:
- Pelvic Exam: A doctor may palpate the abdomen to feel for fibroids.
- Ultrasound: A transabdominal or transvaginal ultrasound provides images of the uterus and fibroids.
- MRI: Offers detailed imaging to plan treatment.
- Hysterosonography: Uses saline infusion during ultrasound to better view the uterine cavity.
- Hysteroscopy: Direct visualization of the uterine lining and fibroids using a small camera inserted into the uterus.
- Blood Tests: To rule out other causes of symptoms, like anemia due to heavy bleeding or hormonal imbalances.
Diagnostic and Treatment Options
a. Diagnostic Tools
- Ultrasound: Non-invasive imaging using sound waves to visualize the uterus and detect fibroids.
- MRI: Provides detailed images of fibroids and their impact on surrounding tissues.
- Hysterosonography: Enhances ultrasound imaging with saline infusion to better view the uterine cavity.
- Hysteroscopy: Involves inserting a small camera into the uterus to directly visualize the uterine lining and fibroids.
b. Treatment Options
- Medications: Hormonal treatments like GnRH agonists can shrink fibroids temporarily. Other medications can manage symptoms but do not eliminate fibroids.
- Non-Invasive Procedures: MRI-guided focused ultrasound surgery (FUS) uses high-frequency sound waves to destroy fibroids.
- Minimally Invasive Procedures:
- Uterine Artery Embolization (UAE): Blocks blood flow to fibroids, causing them to shrink.
- Laparoscopic or Robotic Myomectomy: Removes fibroids through small incisions while preserving the uterus.
- Hysteroscopic Myomectomy: Removes fibroids via the vagina using a hysteroscope.
- Surgical Procedures:
- Hysterectomy: Complete removal of the uterus, which is a permanent solution for fibroids.
- Abdominal Myomectomy: Surgical removal of fibroids through a larger abdominal incision.
c. Alternative and Complementary Therapies
- Diet and Lifestyle Changes: Maintaining a healthy weight, reducing red meat intake, and increasing consumption of green vegetables and fruit may help manage symptoms.
- Herbal Remedies: Some women find relief with herbal treatments, but these should be used with caution and under the guidance of a healthcare provider.
- Acupuncture: Can help manage pain and other symptoms, though evidence is limited.
Living with Uterine Fibroids
Managing fibroids involves more than medical treatment. Here are some tips for living with fibroids:
a. Self-Care Strategies
- Regular Exercise: Helps maintain a healthy weight and reduce symptoms.
- Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, and whole grains.
- Stress Management: Techniques like yoga, meditation, and deep breathing can help manage stress and reduce symptom severity.
b. Support Networks
- Join Support Groups: Connecting with others who have fibroids can provide emotional support and practical advice.
- Educate Yourself: Stay informed about fibroids and treatment options through reputable sources.
Conclusion
Recognizing the early signs and symptoms of uterine fibroids and understanding how to monitor them can empower you to take proactive steps toward managing your health. While self-assessment is valuable, it is not a substitute for professional diagnosis and treatment. Regular self-monitoring and timely consultation with a healthcare provider are crucial for effective management and treatment of uterine fibroids. If you suspect you have fibroids, seek medical advice for a thorough evaluation and appropriate care.
FAQ: How to Check for Uterine Fibroids at Home: Early Signs and Symptoms
Q1: What are uterine fibroids?
A1: Uterine fibroids are benign (non-cancerous) growths that develop from the muscle tissue of the uterus. They vary in size and can be located in different parts of the uterus.
Q2: What are the common symptoms of uterine fibroids?
A2: Common symptoms include:
- Heavy menstrual bleeding
- Prolonged menstrual periods
- Pelvic pain or pressure
- Abdominal swelling or bloating
- Frequent urination
- Difficulty emptying the bladder
- Constipation
- Back and leg pain
- Reproductive issues such as infertility or pregnancy complications
Q3: Can I detect uterine fibroids at home?
A3: While you can monitor symptoms at home, a definitive diagnosis requires a medical examination and imaging tests. Keeping track of your menstrual cycle, noting any pelvic pain, and observing changes in urination and bowel movements can help you recognize potential signs of fibroids.
Q4: How can I track my menstrual cycle and symptoms at home?
A4: Use a period tracking app like Clue or Flo, or a calendar to log:
- Start and end dates of your periods
- Flow intensity and the presence of clots
- Any irregularities, such as spotting or prolonged bleeding
- Associated symptoms like pain or fatigue
Q5: What should I look for when tracking pelvic pain?
A5: Keep a pain diary noting:
- Intensity of the pain on a scale of 1-10
- Location and duration of the pain
- Triggers or factors that alleviate the pain
- Any correlation with your menstrual cycle
Q6: How do I monitor abdominal changes?
A6: Regularly measure your waistline at the same point and note any changes. Observe persistent bloating or visible enlargement that doesn’t fluctuate with diet or digestion.
Q7: What are the signs that fibroids might be affecting my urinary or bowel functions?
A7: Look for:
- Increased frequency of urination or urgency
- Difficulty in completely emptying the bladder
- Chronic constipation or changes in bowel habits
Q8: When should I seek medical help for fibroid symptoms?
A8: Consult a healthcare provider if you experience:
- Persistent heavy or prolonged menstrual bleeding
- Severe pelvic pain or pressure
- Noticeable abdominal swelling
- Frequent urination or difficulty urinating
- Chronic constipation
- Issues with fertility or pregnancy
Q9: What diagnostic tests can confirm the presence of fibroids?
A9: Your doctor may recommend:
- Pelvic Exam: To feel for irregularities in the uterus.
- Ultrasound: To visualize the uterus and identify fibroids.
- MRI: For detailed imaging of fibroids.
- Hysterosonography: Enhanced ultrasound using saline infusion.
- Hysteroscopy: Direct visualization of the uterine cavity with a camera.
Q10: What treatment options are available for uterine fibroids?
A10: Treatments vary based on symptoms, size, and location of fibroids and include:
- Medications: To manage symptoms or shrink fibroids temporarily.
- Non-Invasive Procedures: MRI-guided focused ultrasound surgery.
- Minimally Invasive Procedures: Uterine artery embolization, laparoscopic myomectomy.
- Surgical Procedures: Hysterectomy or abdominal myomectomy.
- Alternative Therapies: Lifestyle changes, dietary adjustments, and stress management.
Q11: Can lifestyle changes help manage fibroid symptoms?
A11: Yes, maintaining a healthy weight, regular exercise, a balanced diet, and stress management techniques like yoga or meditation can help reduce symptoms.
Q12: Are there support networks for women with fibroids?
A12: Yes, joining support groups can provide emotional support and practical advice. Many organizations and online communities offer resources and support for women with fibroids.