Insulin Resistance and PCOS: Connection, Symptoms, and Dietary Solutions
Deep Dive into Insulin Resistance and PCOS
Pathophysiology of Insulin Resistance in PCOS
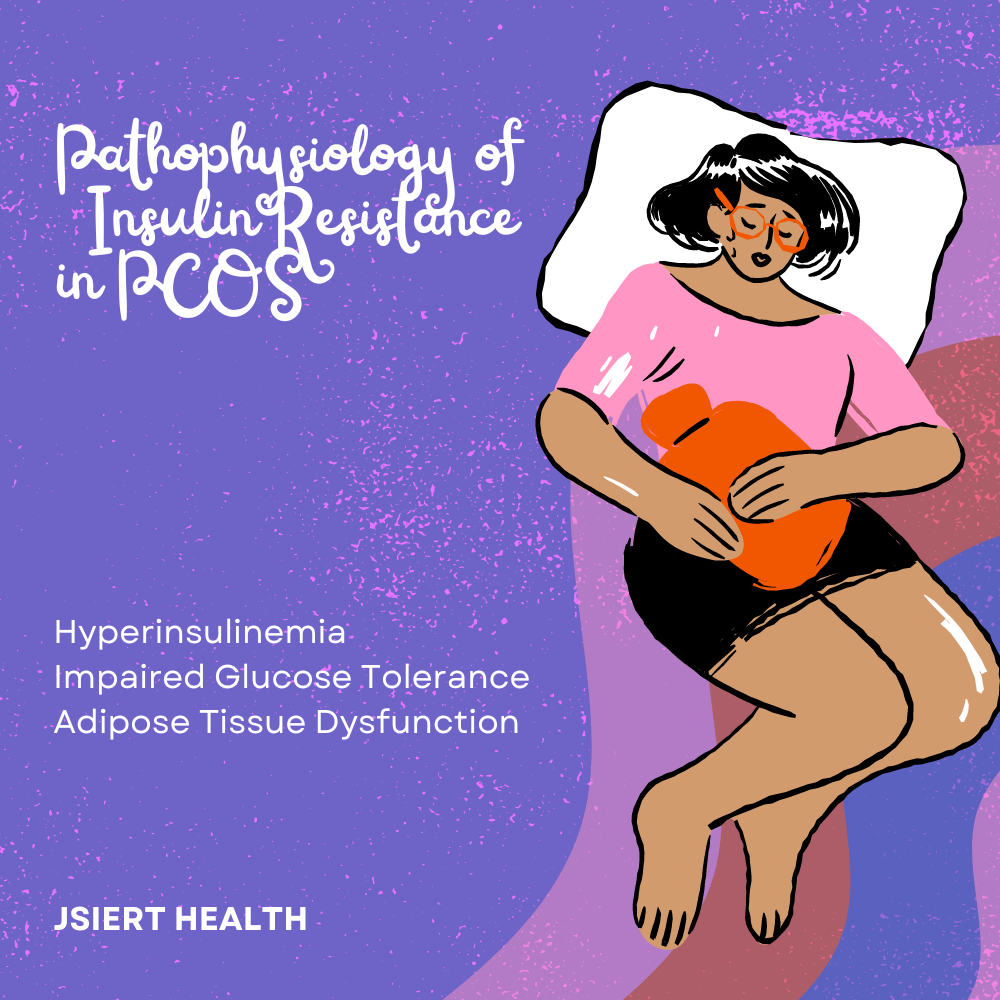
Insulin resistance (IR) is a complex condition where the body’s cells, particularly muscle, fat, and liver cells, do not respond effectively to insulin. This leads to increased insulin production by the pancreas to maintain normal blood glucose levels. High levels of insulin (hyperinsulinemia) further complicate the hormonal landscape in PCOS:
- Hyperinsulinemia: Elevated insulin levels increase androgen production in the ovaries and adrenal glands, exacerbating symptoms like hirsutism and acne.
- Impaired Glucose Tolerance: The body’s inability to use insulin effectively can lead to impaired glucose tolerance and eventually type 2 diabetes if not managed.
- Adipose Tissue Dysfunction: Insulin resistance often leads to central obesity, where fat is primarily stored in the abdominal region, further contributing to metabolic issues.
Detailed Symptoms of Insulin Resistance in PCOS
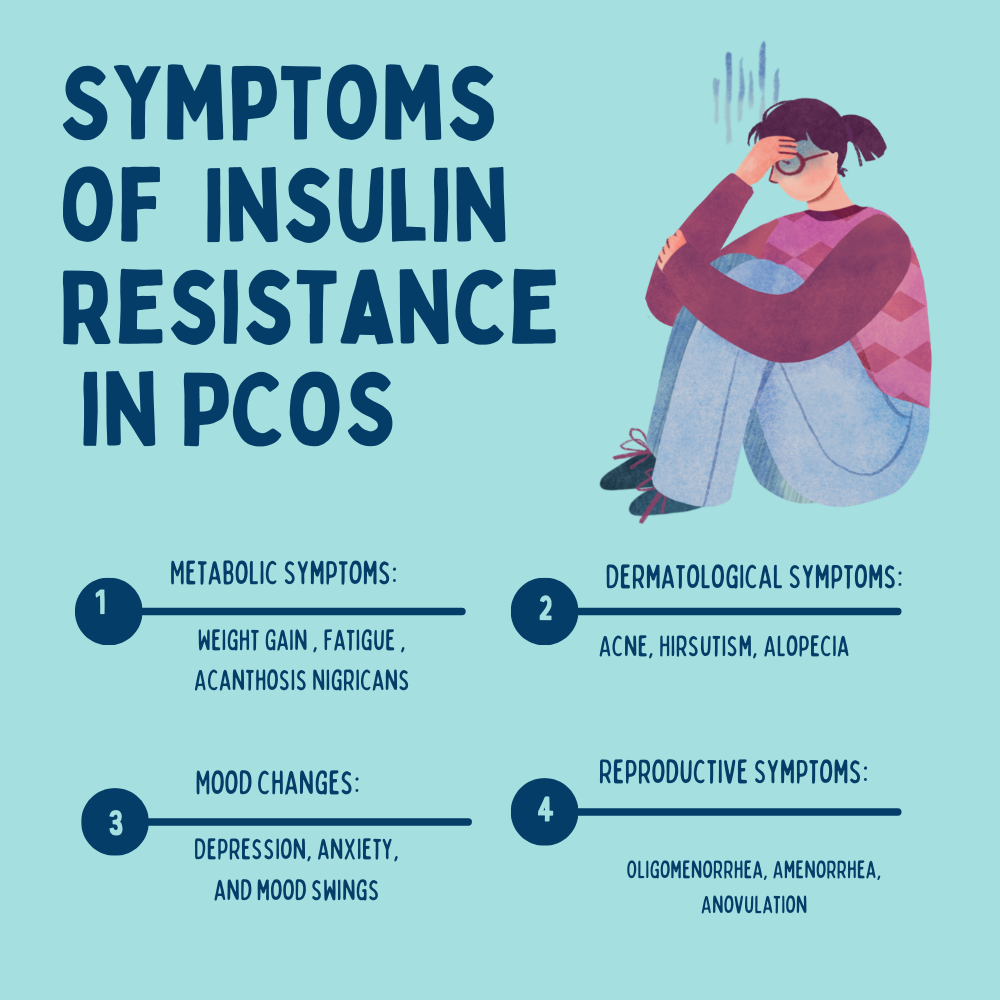
Metabolic Symptoms:
- Weight Gain: Difficulty losing weight or unexplained weight gain, Particularly around the abdomen, due to the body’s impaired ability to metabolize glucose.
- Fatigue: Feeling tired and sluggish, even after a full night’s sleep. Persistent tiredness due to inefficient glucose utilization.
- Acanthosis Nigricans: Dark, velvety patches of skin, typically in body folds and creases.
- Mood changes: Depression, anxiety, and mood swings.
Reproductive Symptoms:
- Oligomenorrhea: Infrequent, irregular, or prolonged menstrual periods.
- Amenorrhea: Absence of menstrual periods.
- Anovulation: Failure to ovulate, leading to fertility issues.
Dermatological Symptoms:
- Hirsutism: Excessive hair growth on the face, chest, and back.
- Acne: Persistent acne, especially in areas like the face, chest, and upper back. Severe, persistent acne resistant to common treatments.
- Alopecia: Thinning of scalp hair or male-pattern baldness.
Comprehensive Dietary Solutions for Insulin Resistance and PCOS

A holistic approach to diet can significantly impact insulin sensitivity and alleviate PCOS symptoms. Here’s an in-depth look at the dietary strategies:
- Low Glycemic Index (GI) Foods:
- Why: Low GI foods are digested and absorbed more slowly, causing a gradual rise in blood glucose and insulin levels.
- Examples:
- Whole Grains: Brown rice, quinoa, barley, whole wheat.
- Legumes: Beans, lentils, chickpeas.
- Fruits: Apples, berries, pears.
- Vegetables: Leafy greens, broccoli, cauliflower.
- Nuts: Almonds, walnuts, cashews.
- Balanced Macronutrients:
- Why: A balanced intake of macronutrients helps maintain steady blood sugar levels and supports overall health.
- Examples:
- Proteins: Chicken, fish, eggs, tofu, beans.
- Fats: Olive oil, avocado, nuts, seeds.
- Carbohydrates: Whole grains, starchy vegetables.
- Increase Fiber Intake:
- Why: Fiber helps regulate blood sugar by slowing down digestion and absorption of carbohydrates.
- Examples:
- Vegetables: Brussels sprouts, carrots, spinach.
- Fruits: Berries, oranges, apples.
- Whole Grains: Oats, brown rice, whole wheat.
- Legumes: Lentils, black beans, kidney beans.
- Nuts and Seeds: Chia seeds, flaxseeds, almonds.
- Reduce Refined Carbohydrates and Sugars:
- Why: Refined carbs and sugars can cause rapid spikes in blood sugar and insulin levels, leading to insulin resistance.
- What to Avoid:
- Sugary drinks (soda, fruit juices).
- Sweets and desserts (cakes, cookies, candy).
- White bread, white rice, and other refined grains.
- Processed snacks (chips, crackers).
- Healthy Fats:
- Why: Healthy fats improve insulin sensitivity and provide a steady source of energy.
- Examples:
- Fatty Fish: Salmon, mackerel, sardines.
- Avocado: Rich in monounsaturated fats.
- Nuts: Almonds, walnuts, pecans.
- Seeds: Chia seeds, flaxseeds, pumpkin seeds.
- Oils: Olive oil, coconut oil.
- Regular Meals and Snacks:
- Why: Consistent eating patterns help maintain stable blood sugar levels.
- What to Do:
- Eat small, balanced meals every 3-4 hours.
- Include a mix of protein, healthy fats, and fiber in each meal/snack.
- Stay Hydrated:
- Why: Proper hydration supports metabolic processes and overall health.
- What to Do:
- Drink at least 8 glasses of water daily.
- Limit sugary drinks and caffeinated beverages.
Detailed Example Meal Plan for Insulin Resistance and PCOS
Breakfast:
- Oatmeal: Cooked with water or unsweetened almond milk, topped with fresh berries, a handful of nuts (walnuts or almonds), and a drizzle of honey.
- Drink: Green tea or water.
Morning Snack:
- Greek Yogurt: Plain, unsweetened, with a handful of mixed nuts (almonds, walnuts, cashews).
Lunch:
- Grilled Chicken Salad: Mixed greens, cherry tomatoes, cucumbers, bell peppers, and a vinaigrette dressing made with olive oil and lemon juice.
- Whole Grain Roll: Optional, for additional fiber.
Afternoon Snack:
- Apple Slices: With a tablespoon of almond butter.
Dinner:
- Baked Salmon: Seasoned with herbs and lemon.
- Quinoa: Cooked with vegetable broth.
- Steamed Broccoli: Drizzled with olive oil.
- Mixed Green Salad: With olive oil and lemon dressing.
Evening Snack:
- Carrot Sticks: With hummus.
Additional Lifestyle Tips

Regular Exercise:
- Why: Physical activity enhances insulin sensitivity, helps with weight management, and improves overall health.
- What to Do:
- Aim for at least 150 minutes of moderate aerobic exercise per week (e.g., brisk walking, cycling, swimming).
- Incorporate strength training exercises at least twice a week to build muscle mass and improve metabolism.
Stress Management:
- Why: Chronic stress can exacerbate insulin resistance and hormonal imbalances.
- What to Do:
- Practice relaxation techniques such as yoga, meditation, deep breathing exercises.
- Engage in hobbies and activities that you enjoy to reduce stress.
Adequate Sleep:
- Why: Poor sleep quality can worsen insulin resistance and negatively impact hormonal balance.
- What to Do:
- Aim for 7-9 hours of quality sleep per night.
- Establish a regular sleep routine and create a relaxing bedtime environment.
- Avoid caffeine and heavy meals close to bedtime.
Regular Health Monitoring:
- Why: Regular monitoring helps in early detection and management of any health issues related to PCOS and insulin resistance.
- What to Do:
- Regularly check blood sugar levels.
- Monitor weight and waist circumference.
- Have periodic blood tests to monitor cholesterol levels, triglycerides, and hormone levels.
- Visit your healthcare provider regularly for comprehensive check-ups.
By implementing these detailed dietary strategies and lifestyle modifications, women with PCOS can better manage insulin resistance, alleviate symptoms, and improve their overall quality of life.
FAQ for Insulin Resistance and PCOS: Connection, Symptoms, and Dietary Solutions
1. What is the connection between insulin resistance and PCOS?
Answer: Insulin resistance (IR) is a condition where the body’s cells become less responsive to insulin, leading to higher levels of insulin in the blood. In women with PCOS, elevated insulin levels can stimulate the ovaries to produce more androgens (male hormones), which can exacerbate PCOS symptoms such as hirsutism, acne, and irregular menstrual cycles. Insulin resistance is also associated with weight gain, particularly around the abdomen, which can further complicate PCOS.
2. What are the common symptoms of insulin resistance in women with PCOS?
Answer: Common symptoms include:
- Irregular menstrual cycles
- Excessive hair growth (hirsutism)
- Acne and oily skin
- Weight gain, especially around the abdomen
- Dark, velvety skin patches (acanthosis nigricans)
- Fatigue and low energy levels
- Mood swings, anxiety, and depression
3. How does diet impact insulin resistance and PCOS?
Answer: Diet plays a crucial role in managing insulin resistance and PCOS. Consuming a balanced diet that includes low glycemic index foods, high fiber, and healthy fats can help stabilize blood sugar levels and improve insulin sensitivity. Avoiding refined carbohydrates and sugars can prevent blood sugar spikes and reduce insulin levels.
4. What foods should be included in a diet for managing insulin resistance and PCOS?
Answer: Foods to include are:
- Low GI Foods: Whole grains, legumes, fruits (berries, apples), vegetables (leafy greens, broccoli), and nuts.
- High-Fiber Foods: Vegetables, fruits, whole grains, legumes, nuts, and seeds.
- Healthy Fats: Avocados, olive oil, nuts, seeds, and fatty fish (salmon, mackerel).
- Lean Proteins: Chicken, fish, eggs, tofu, and legumes.
5. What foods should be avoided to manage insulin resistance and PCOS?
Answer: Avoid:
- Refined sugars and sweets (cakes, candies, pastries)
- Sugary drinks (soda, fruit juices)
- Refined grains (white bread, white rice)
- Processed snacks (chips, crackers)
6. How can regular meals and snacks help with insulin resistance and PCOS?
Answer: Eating regular meals and snacks helps maintain stable blood sugar levels throughout the day, preventing spikes and crashes that can worsen insulin resistance. It is important to eat small, balanced meals every 3-4 hours, including a mix of protein, healthy fats, and fiber.
7. What lifestyle changes can help manage insulin resistance and PCOS?
Answer: Key lifestyle changes include:
- Regular Exercise: At least 150 minutes of moderate aerobic exercise per week and strength training twice a week.
- Stress Management: Techniques like yoga, meditation, and deep breathing can help reduce stress levels.
- Adequate Sleep: Aim for 7-9 hours of quality sleep per night. Establish a regular sleep routine and create a relaxing bedtime environment.
- Regular Health Monitoring: Regular check-ups with a healthcare provider to monitor blood sugar levels, cholesterol, and overall health.
8. Can losing weight help with insulin resistance and PCOS?
Answer: Yes, losing weight can significantly improve insulin sensitivity and help regulate menstrual cycles, reduce androgen levels, and alleviate PCOS symptoms. Even a modest weight loss of 5-10% of body weight can have a positive impact.
9. Are there any specific supplements that can help with insulin resistance and PCOS?
Answer: Some supplements that may help include:
- Inositol: Particularly myo-inositol, which can improve insulin sensitivity and reduce symptoms of PCOS.
- Vitamin D: Deficiency is common in women with PCOS, and supplementation can improve insulin resistance.
- Omega-3 Fatty Acids: Found in fish oil, can reduce inflammation and improve insulin sensitivity.
- Chromium: May help improve blood sugar control.
Always consult with a healthcare provider before starting any new supplement regimen.
10. How does stress impact insulin resistance and PCOS?
Answer: Stress can increase the production of cortisol, a hormone that can worsen insulin resistance. Chronic stress can also disrupt sleep and lead to unhealthy eating habits, further complicating the management of PCOS. Stress-reducing techniques such as yoga, meditation, and regular physical activity can help mitigate these effects.