Optimizing Your Diet for PCOD and PCOS: Expert Recommendations and Meal Plans
Optimizing Your Diet for PCOD and PCOS: Expert Recommendations and Meal Plans
Introduction:
- Brief Overview of PCOD and PCOS:
- Polycystic ovary syndrome (PCOS) and polycystic ovary disorder (PCOD) are common endocrine disorders affecting women of reproductive age.
- PCOS is characterized by hormonal imbalances, irregular menstrual cycles, and the presence of cysts on the ovaries.
- PCOD shares similar symptoms with PCOS but may present differently in terms of severity and manifestation.
- Both conditions can lead to various health complications, including infertility, insulin resistance, obesity, and cardiovascular issues.
- Importance of Diet in Managing Symptoms:
- Diet plays a crucial role in the management of PCOD and PCOS by influencing hormone levels, insulin sensitivity, and inflammation.
- Certain dietary patterns can exacerbate symptoms, while others can help alleviate them and improve overall well-being.
- Proper nutrition can aid in weight management, regulate menstrual cycles, reduce the risk of complications, and enhance fertility outcomes.
- Implementing dietary changes is often recommended as a primary or adjunctive therapy alongside medical interventions for optimal symptom control.
- Purpose of the Guide:
- This guide aims to provide comprehensive and evidence-based recommendations for optimizing diet in individuals with PCOD and PCOS.
- By offering expert insights and practical meal plans, the guide seeks to empower individuals to make informed dietary choices that support their health goals.
- Through a holistic approach that integrates nutrition, lifestyle modifications, and potential supplementation, the guide aims to address the multifaceted nature of PCOD and PCOS management.
- Ultimately, the guide aspires to help individuals with PCOD and PCOS achieve better symptom control, hormonal balance, and overall quality of life through optimized dietary practices.
Understanding PCOD and PCOS:
- Definition and Differences between PCOD and PCOS:
- Polycystic ovary disorder (PCOD) and polycystic ovary syndrome (PCOS) are both endocrine disorders affecting the ovaries.
- PCOD is characterized by multiple small cysts on the ovaries, irregular menstrual cycles, and hormonal imbalances, without meeting all the criteria for PCOS.
- PCOS is a more severe form, defined by the presence of cysts on the ovaries, irregular menstrual cycles, and hormonal imbalances, often accompanied by symptoms such as excess hair growth, acne, and obesity.
- While PCOD and PCOS share similarities, PCOS typically involves more pronounced symptoms and increased risk of complications.
- Causes, Symptoms, and Potential Complications:
- The exact cause of PCOD and PCOS is not fully understood, but genetic, environmental, and lifestyle factors are believed to play significant roles.
- Common symptoms include irregular menstrual cycles, excess hair growth (hirsutism), acne, weight gain, and infertility.
- Potential complications of PCOD and PCOS include infertility, insulin resistance, type 2 diabetes, cardiovascular disease, and endometrial cancer.
- Hormonal imbalances, particularly elevated levels of androgens (male hormones) and insulin, contribute to the manifestation of symptoms and complications.
- Importance of Hormonal Balance and Insulin Sensitivity:
- Hormonal balance, particularly of estrogen, progesterone, and androgens, is crucial for normal ovarian function and menstrual cycle regulation.
- Imbalances in these hormones, such as elevated levels of testosterone, can disrupt ovulation, leading to irregular menstrual cycles and fertility issues.
- Insulin resistance, a hallmark feature of PCOD and PCOS, occurs when cells become less responsive to insulin, leading to elevated insulin levels in the blood.
- Insulin resistance exacerbates hormonal imbalances, promotes excess androgen production, and contributes to metabolic disturbances, such as weight gain and dyslipidemia.
- Optimizing hormonal balance and improving insulin sensitivity through diet and lifestyle interventions are key strategies for managing symptoms and reducing the risk of complications in individuals with PCOD and PCOS.
The Role of Diet in PCOD and PCOS Management:

- Impact of Diet on Hormone Levels and Inflammation:
- Diet plays a significant role in modulating hormone levels, including insulin, estrogen, progesterone, and androgens, all of which are implicated in PCOD and PCOS.
- Certain dietary factors can exacerbate hormonal imbalances and inflammation, worsening symptoms and contributing to metabolic dysfunction.
- High intake of refined carbohydrates, sugars, and processed foods can lead to spikes in blood sugar levels, triggering insulin secretion and promoting insulin resistance.
- Insulin resistance, in turn, stimulates the ovaries to produce excess androgens, such as testosterone, exacerbating symptoms like hirsutism, acne, and irregular menstrual cycles.
- Chronic inflammation, driven by poor dietary choices, can further disrupt hormonal balance and exacerbate symptoms associated with PCOD and PCOS.
- Conversely, adopting a diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can help reduce inflammation and mitigate the impact of hormonal imbalances.
- Relationship Between Diet and Insulin Resistance:
- Insulin resistance is a central feature of PCOD and PCOS, characterized by impaired response of cells to insulin, leading to elevated insulin levels in the blood.
- Dietary factors that contribute to insulin resistance include excessive intake of refined carbohydrates, sugars, and saturated fats, which can lead to chronically elevated blood sugar and insulin levels.
- Insulin resistance exacerbates hormonal imbalances by promoting excess androgen production, disrupting ovulation, and contributing to weight gain and metabolic disturbances.
- Adopting a diet that promotes insulin sensitivity is crucial for managing PCOD and PCOS symptoms and reducing the risk of complications.
- Dietary strategies to improve insulin sensitivity include focusing on whole, unprocessed foods, emphasizing fiber-rich carbohydrates, incorporating lean proteins, and including healthy fats in moderation.
- Balancing macronutrients and avoiding excessive calorie intake can also help improve insulin sensitivity and promote metabolic health in individuals with PCOD and PCOS.
- Introduction to Glycemic Index/Load and Its Relevance:
- The glycemic index (GI) is a measure of how quickly carbohydrates in food raise blood sugar levels after consumption.
- Foods with a high GI cause a rapid spike in blood sugar, followed by a sharp drop, which can exacerbate insulin resistance and promote hormonal imbalances.
- The glycemic load (GL) takes into account both the quality and quantity of carbohydrates in a serving of food, providing a more accurate reflection of its impact on blood sugar levels.
- Choosing low-GI and low-GL foods can help stabilize blood sugar levels, improve insulin sensitivity, and support hormone balance in individuals with PCOD and PCOS.
- Examples of low-GI foods include non-starchy vegetables, legumes, whole grains, and fruits with a low sugar content, while high-GI foods include refined grains, sugary snacks, and processed foods.
- Incorporating low-GI and low-GL foods into meals and snacks can help regulate blood sugar levels, reduce insulin resistance, and support overall metabolic health in individuals with PCOD and PCOS.
Expert Recommendations for PCOD and PCOS Diet:
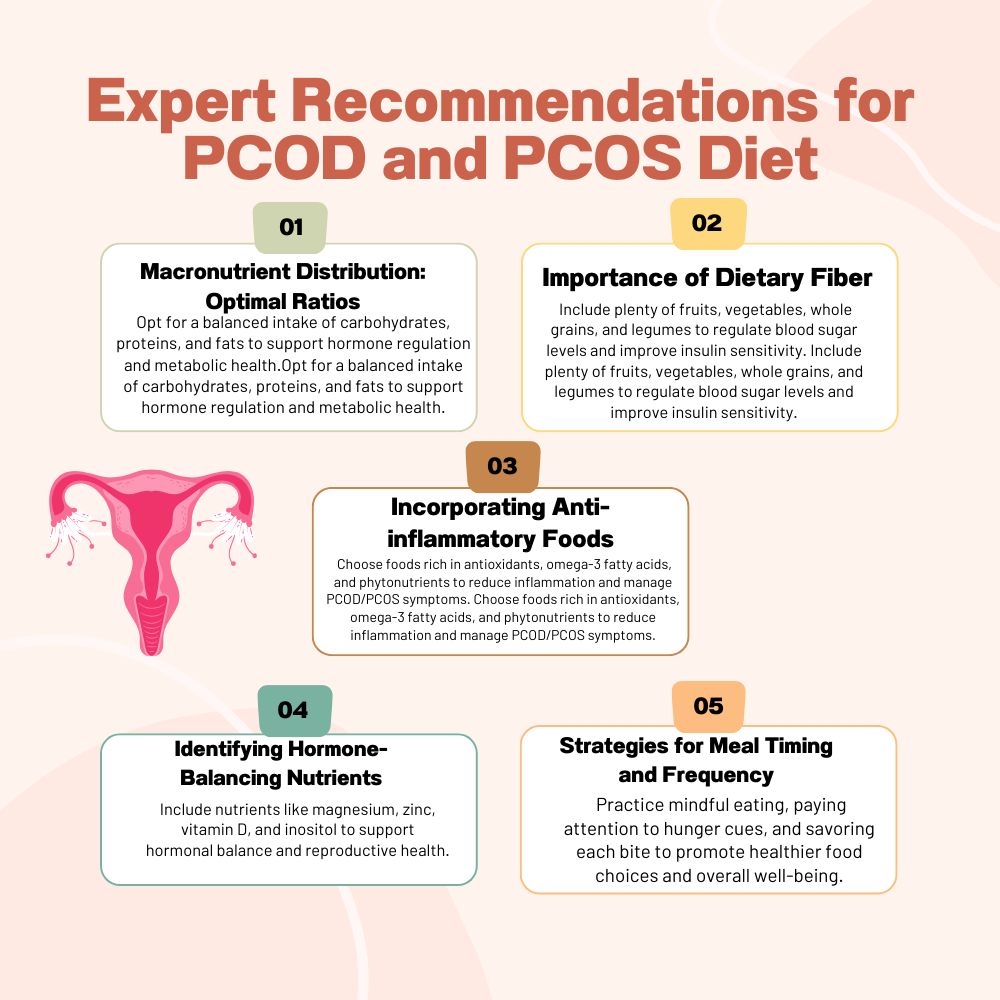
- Macronutrient Distribution: Optimal Ratios:
- The optimal macronutrient distribution for individuals with PCOD and PCOS typically includes a balanced ratio of carbohydrates, proteins, and fats.
- A common recommendation is to aim for a macronutrient distribution of approximately 40-50% carbohydrates, 25-35% protein, and 25-35% fat.
- Carbohydrates should primarily come from complex sources such as whole grains, legumes, fruits, and vegetables, which provide sustained energy and fiber to help regulate blood sugar levels.
- Proteins should be lean and include sources such as poultry, fish, tofu, legumes, and dairy products, which support muscle health and satiety.
- Healthy fats, including monounsaturated and polyunsaturated fats from sources like avocados, nuts, seeds, and olive oil, are important for hormone production and absorption of fat-soluble vitamins.
- Importance of Dietary Fiber:
- Dietary fiber plays a crucial role in PCOD and PCOS management by promoting satiety, regulating blood sugar levels, and supporting gut health.
- Adequate fiber intake can help prevent spikes in blood sugar levels, reduce insulin resistance, and promote weight management.
- Aim for a variety of fiber-rich foods, including fruits, vegetables, whole grains, legumes, nuts, and seeds, to ensure adequate intake.
- Soluble fiber, found in foods like oats, barley, beans, and apples, can help lower cholesterol levels and stabilize blood sugar levels.
- Insoluble fiber, found in foods like whole grains, nuts, seeds, and vegetables, adds bulk to the stool and supports digestive health.
- Incorporating Anti-inflammatory Foods:
- Anti-inflammatory foods can help reduce inflammation, which is often elevated in individuals with PCOD and PCOS.
- Focus on incorporating foods rich in antioxidants, vitamins, minerals, and phytonutrients, which have anti-inflammatory properties.
- Examples of anti-inflammatory foods include colorful fruits and vegetables, fatty fish rich in omega-3 fatty acids (such as salmon, mackerel, and sardines), nuts, seeds, olive oil, turmeric, ginger, and green tea.
- Limit intake of pro-inflammatory foods such as processed meats, refined carbohydrates, sugary snacks, and trans fats, which can exacerbate inflammation and worsen PCOD and PCOS symptoms.
- Identifying Hormone-Balancing Nutrients:
- Certain nutrients play a role in hormone regulation and can help balance hormone levels in individuals with PCOD and PCOS.
- Key hormone-balancing nutrients include magnesium, zinc, vitamin D, omega-3 fatty acids, and inositol.
- Magnesium-rich foods include leafy greens, nuts, seeds, and whole grains, while zinc is found in meat, shellfish, legumes, nuts, and seeds.
- Vitamin D can be obtained from sunlight exposure and fortified foods such as fatty fish, eggs, and fortified dairy products.
- Omega-3 fatty acids are found in fatty fish, flaxseeds, chia seeds, walnuts, and hemp seeds, and can help reduce inflammation and support hormone balance.
- Inositol, a B-vitamin-like compound, is found in foods such as beans, citrus fruits, and whole grains, and may help improve insulin sensitivity and ovarian function in women with PCOS.
- Strategies for Meal Timing and Frequency:
- Consistent meal timing and frequency can help stabilize blood sugar levels, regulate appetite, and support hormone balance.
- Aim for balanced meals containing a combination of carbohydrates, proteins, and fats every 3-4 hours throughout the day to maintain steady energy levels and prevent spikes in blood sugar.
- Avoid skipping meals or going for long periods without eating, as this can lead to overeating, blood sugar fluctuations, and hormonal imbalances.
- Pay attention to portion sizes and listen to your body’s hunger and satiety cues to avoid overeating and promote mindful eating habits.
- Experiment with meal timing and frequency to find a pattern that works best for your individual needs and preferences, while keeping in mind the importance of consistency and balance in PCOD and PCOS management.
Lifestyle Factors and PCOD/PCOS Management:
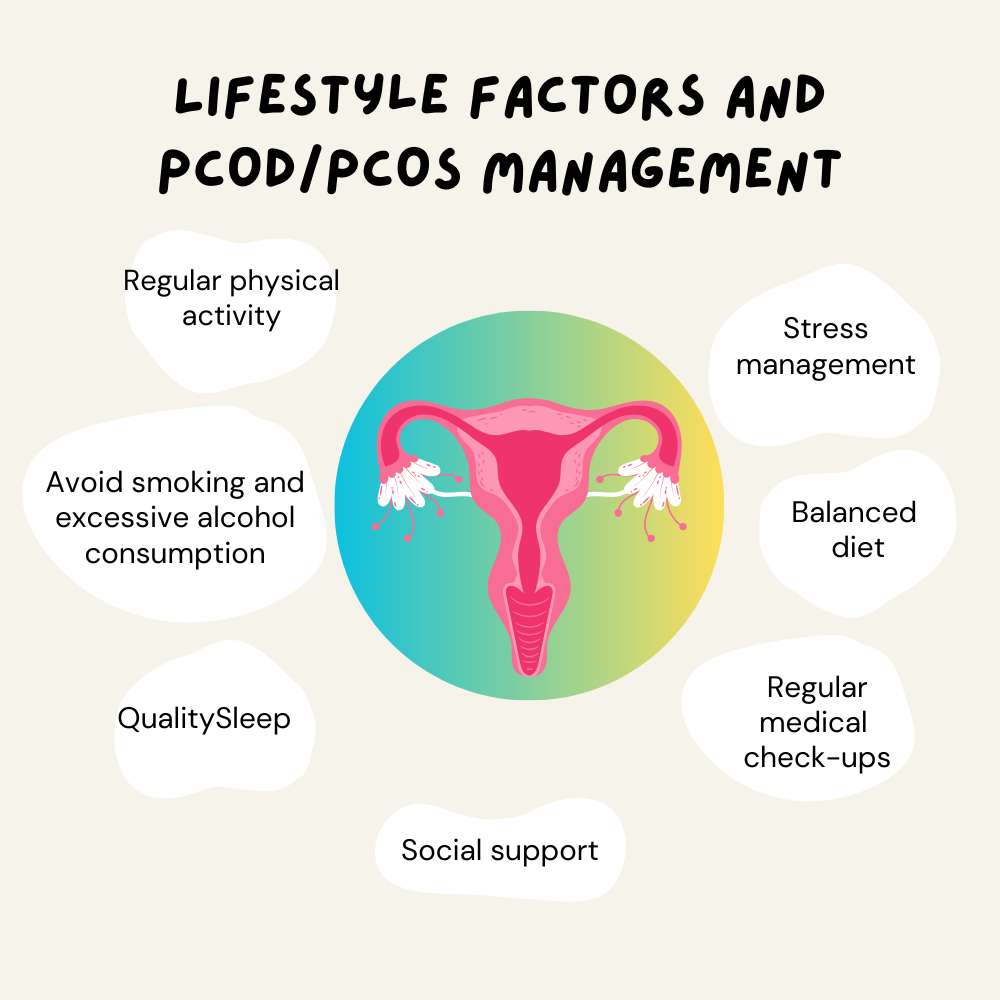
- Role of Physical Activity, Stress Management, and Sleep:
- Physical activity plays a crucial role in managing PCOD and PCOS by improving insulin sensitivity, promoting weight loss, and reducing stress.
- Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, swimming, or dancing, to support overall health and hormone balance.
- Incorporate strength training exercises 2-3 times per week to build lean muscle mass, which can help increase metabolism and improve insulin sensitivity.
- Stress management techniques such as mindfulness meditation, deep breathing exercises, yoga, and progressive muscle relaxation can help reduce cortisol levels and alleviate symptoms associated with PCOD and PCOS.
- Prioritize quality sleep, aiming for 7-9 hours per night, as inadequate sleep can disrupt hormone levels, increase stress, and exacerbate symptoms of PCOD and PCOS.
- Establish a regular sleep schedule, create a relaxing bedtime routine, and create a conducive sleep environment to promote restful sleep and support overall well-being.
- Importance of Holistic Approach to Health:
- Adopting a holistic approach to health is essential for effectively managing PCOD and PCOS and optimizing overall well-being.
- This approach encompasses dietary changes, physical activity, stress management, sleep hygiene, and other lifestyle factors that impact health.
- Recognize the interconnectedness of physical, mental, and emotional health, and strive to address all aspects of well-being for comprehensive PCOD and PCOS management.
- Engage in activities that promote relaxation, enjoyment, and fulfillment, such as hobbies, socializing with loved ones, and spending time in nature.
- Cultivate a positive mindset and practice self-compassion, understanding that managing PCOD and PCOS is a journey that requires patience, perseverance, and self-care.
- Seek support from healthcare professionals, support groups, and online communities to navigate challenges, stay motivated, and access resources for PCOD and PCOS management.
- Remember that every individual is unique, and it may take time to find the combination of lifestyle factors that works best for you. Be open to experimentation, adaptation, and continuous learning on your journey to optimized health with PCOD and PCOS.
Supplements and Nutraceuticals:
- Overview of Supplements such as Inositol, Omega-3 Fatty Acids, and Vitamin D:
- Inositol: Inositol is a naturally occurring compound that belongs to the vitamin B family. It has been studied for its potential benefits in managing PCOD and PCOS symptoms, particularly in improving insulin sensitivity, ovarian function, and menstrual regularity. Inositol supplements are available in two forms: myo-inositol and D-chiro-inositol.
- Omega-3 Fatty Acids: Omega-3 fatty acids, including Eicosapentaenoic Acid ( EPA ) and Docosahexaenoic acid (DHA), are essential fatty acids found in fatty fish, flaxseeds, chia seeds, and walnuts. They have anti-inflammatory properties and may help reduce inflammation, improve insulin sensitivity, and support hormonal balance in individuals with PCOD and PCOS.
- Vitamin D: Vitamin D is a fat-soluble vitamin that plays a crucial role in bone health, immune function, and hormone regulation. Low vitamin D levels are common in individuals with PCOD and PCOS and have been associated with insulin resistance, menstrual irregularities, and other symptoms. Supplementing with vitamin D may help improve insulin sensitivity and reproductive outcomes in women with PCOS.
- Scientific Evidence Supporting Their Use:
- Inositol: Numerous clinical studies have demonstrated the efficacy of inositol supplementation in improving insulin sensitivity, reducing androgen levels, restoring menstrual regularity, and promoting ovulation in women with PCOS. Both myo-inositol and D-chiro-inositol have been shown to be effective, either alone or in combination.
- Omega-3 Fatty Acids: Research suggests that omega-3 fatty acids may help reduce inflammation, improve lipid profiles, and lower androgen levels in women with PCOD and PCOS. Some studies have also reported improvements in menstrual regularity and ovulation with omega-3 supplementation, although further research is needed to confirm these findings.
- Vitamin D: Studies have shown that vitamin D supplementation may improve insulin sensitivity, menstrual regularity, and fertility outcomes in women with PCOS. Adequate vitamin D levels have also been associated with a reduced risk of developing metabolic complications such as type 2 diabetes and cardiovascular disease in women with PCOS.
- Considerations for Supplement Use:
- Before starting any supplement regimen, it’s important to consult with a healthcare provider, particularly a physician or registered dietitian familiar with PCOD and PCOS management.
- Supplements should be used as adjunctive therapies alongside dietary and lifestyle interventions, not as replacements for healthy habits.
- Dosage recommendations for supplements may vary depending on individual factors such as age, weight, medical history, and vitamin/mineral status. It’s essential to follow recommended dosage guidelines and avoid exceeding safe limits.
- Quality and purity of supplements are crucial. Choose reputable brands that undergo third-party testing for potency, purity, and safety.
- Monitor for any potential side effects or interactions with medications when using supplements, and discontinue use if adverse reactions occur.
- Incorporating a variety of nutrient-rich foods into the diet remains the foundation of PCOD and PCOS management, with supplements used as complementary strategies to address specific nutritional needs or deficiencies.
Navigating Challenges and Roadblocks:
- Common Obstacles and Misconceptions:
- Lack of Awareness: Many individuals with PCOD and PCOS may not fully understand their condition or the role of diet in managing symptoms. This can lead to confusion, frustration, and difficulty implementing dietary changes.
- Dietary Restrictions: Adopting a PCOD/PCOS-friendly diet may seem restrictive or overwhelming, particularly if individuals are accustomed to certain eating habits or cultural food preferences.
- Emotional Eating: Emotional factors such as stress, anxiety, and depression can contribute to emotional eating behaviors, leading to cravings for unhealthy foods and difficulty sticking to a balanced diet.
- Social Pressures: Social situations, gatherings, and events often revolve around food, making it challenging to adhere to dietary recommendations and resist temptations.
- Misconceptions: There are several misconceptions surrounding PCOD/PCOS and diet, such as the belief that weight loss is the only goal or that certain foods are strictly off-limits without considering individual needs and preferences.
- Strategies for Overcoming Challenges:
- Education and Awareness: Providing comprehensive education about PCOD/PCOS and the role of diet in managing symptoms can empower individuals to make informed choices and overcome misconceptions.
- Individualized Approach: Recognize that each person’s journey with PCOD/PCOS is unique, and dietary recommendations should be tailored to individual needs, preferences, and health goals.
- Gradual Changes: Instead of making drastic dietary changes overnight, encourage gradual modifications and small, sustainable steps towards healthier eating habits.
- Support System: Building a support network of healthcare professionals, family members, friends, or online communities can provide encouragement, accountability, and practical tips for navigating challenges.
- Mindful Eating: Encourage mindful eating practices, such as paying attention to hunger and fullness cues, savoring flavors and textures, and practicing non-judgmental awareness of thoughts and emotions related to food.
- Meal Planning and Preparation: Planning meals ahead of time, batch cooking, and preparing healthy snacks can help individuals stay on track with their dietary goals and avoid impulsive food choices.
- Coping Strategies: Develop coping strategies for managing stress, emotions, and cravings without turning to food, such as engaging in relaxation techniques, hobbies, or physical activities.
- Flexibility and Moderation: Emphasize flexibility and moderation rather than strict adherence to dietary rules. Allow for occasional indulgences or deviations from the plan while focusing on overall balance and consistency.
- Celebrate Successes: Celebrate achievements, no matter how small, and acknowledge progress towards healthier eating habits and improved well-being. Positive reinforcement can help maintain motivation and momentum on the journey to optimizing diet for PCOD and PCOS.
Conclusion:
In conclusion, optimizing your diet for PCOD and PCOS is a multifaceted journey that requires careful consideration, dedication, and perseverance. Throughout this guide, we have explored various aspects of diet and lifestyle interventions aimed at managing symptoms, promoting hormonal balance, and improving overall well-being for individuals with PCOD and PCOS. Let’s recap some key points:
- Understanding PCOD and PCOS: We delved into the definitions, differences, causes, symptoms, and potential complications of PCOD and PCOS, highlighting the importance of hormonal balance and insulin sensitivity in these conditions.
- The Role of Diet: We discussed how diet influences hormone levels, inflammation, and insulin resistance, emphasizing the significance of macronutrient distribution, dietary fiber, anti-inflammatory foods, and hormone-balancing nutrients.
- Lifestyle Factors: We explored the role of physical activity, stress management, sleep, and adopting a holistic approach to health in PCOD and PCOS management, recognizing the interconnectedness of these factors with dietary choices.
- Supplements and Nutraceuticals: We provided an overview of supplements such as inositol, omega-3 fatty acids, and vitamin D, along with the scientific evidence supporting their use as adjunctive therapies in PCOD and PCOS management.
- Navigating Challenges: We addressed common obstacles, misconceptions, and strategies for overcoming challenges on the journey to optimizing diet for PCOD and PCOS, emphasizing education, individualization, support, and mindful eating practices.
In closing, I want to encourage you to take the information provided in this guide and implement it into your daily life. Making dietary changes can be challenging, but it’s important to remember that small steps can lead to significant improvements in your health over time. Be patient with yourself, stay persistent, and celebrate your successes along the way. Remember that you’re not alone on this journey, and support is available from healthcare professionals, support groups, and online communities. By prioritizing your health and well-being and adopting a balanced approach to nutrition and lifestyle, you can take control of your PCOD and PCOS and enhance your quality of life.
References:
- Arentz S, Abbott JA, Smith CA, Bensoussan A. Herbal medicine for the management of polycystic ovary syndrome (PCOS) and associated oligo/amenorrhoea and hyperandrogenism; a review of the laboratory evidence for effects with corroborative clinical findings. BMC Complement Altern Med. 2014;14:511. doi:10.1186/1472-6882-14-511
- Pal L, Berry A, Coraluzzi L, et al. Therapeutic implications of vitamin D and calcium in overweight women with polycystic ovary syndrome. Gynecol Endocrinol. 2012;28(12):965-968. doi:10.3109/09513590.2012.688912
- Thys-Jacobs S, Starkey P, Bernstein D, Tian J. Calcium carbonate and the premenstrual syndrome: effects on premenstrual and menstrual symptoms. Premenstrual Syndrome Study Group. Am J Obstet Gynecol. 1998;179(2):444-452. doi:10.1016/s0002-9378(98)70344-4
- Günalan E, Yaba A, Yaba D, Ekici S, Özaydın AN. Effects of resveratrol on ovarian morphology, plasma anti-Müllerian hormone, IGF-1 levels, and oxidative stress parameters in a rat model of polycystic ovary syndrome. Reprod Sci. 2020;27(6):1286-1294. doi:10.1007/s43032-020-00178-1
- Mier-Cabrera J, Aburto-Soto T, Burrola-Méndez S, et al. Women with polycystic ovary syndrome secrete higher levels of circulating visfatin, a marker of insulin resistance: a pilot study. Med Sci Monit. 2010;16(8):CR375-380.
- Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011;(7):CD007506. doi:10.1002/14651858.CD007506.pub2
- Palomba S, Falbo A, Zullo F, Orio F Jr. Evidence-based and potential benefits of metformin in the polycystic ovary syndrome: a comprehensive review. Endocr Rev. 2009;30(1):1-50. doi:10.1210/er.2008-0030
- Teede HJ, Misso ML, Costello MF, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602-1618. doi:10.1093/humrep/dey256
- Thakkar S, Patel P. Polycystic ovary syndrome and diet: A review of guidelines, dietary approaches, and dietary supplements. Clin Dermatol. 2019;37(6):608-614. doi:10.1016/j.clindermatol.2019.07.007
- Yarizadeh H, Shokrpour M, Mirmohammadali M, Nouri M. The effect of vitamin D and calcium plus vitamin D on menstrual cycle, body mass index and hyperandrogenism state of women with poly cystic ovarian syndrome. J Clin Diagn Res. 2017;11(5):QC13-QC16. doi:10.7860/JCDR/2017/26733.9881
FAQ for Optimizing Your Diet for PCOD and PCOS:
- What is PCOD and PCOS?
- PCOD (Polycystic Ovary Disorder) and PCOS (Polycystic Ovary Syndrome) are common endocrine disorders characterized by hormonal imbalances, irregular menstrual cycles, and ovarian cysts.
- How does diet affect PCOD and PCOS?
- Diet plays a crucial role in managing symptoms of PCOD and PCOS by influencing hormone levels, insulin sensitivity, inflammation, and overall metabolic health.
- What are some dietary recommendations for PCOD and PCOS?
- Recommended dietary strategies include balancing macronutrients, consuming fiber-rich foods, incorporating anti-inflammatory foods, and identifying hormone-balancing nutrients.
- Can supplements help manage PCOD and PCOS?
- Certain supplements such as inositol, omega-3 fatty acids, and vitamin D may offer benefits in managing symptoms and supporting overall health in individuals with PCOD and PCOS.
- What lifestyle factors are important for PCOD and PCOS management?
- Lifestyle factors such as regular physical activity, stress management, quality sleep, and adopting a holistic approach to health are essential components of PCOD and PCOS management.
- How can I overcome challenges in optimizing my diet for PCOD and PCOS?
- Overcoming challenges may involve education, individualized approaches, gradual changes, building a support system, practicing mindful eating, and seeking guidance from healthcare professionals.
- Are there any specific meal plans or recipes available?
- While specific meal plans and recipes may vary based on individual needs and preferences, incorporating balanced meals with a variety of nutrient-rich foods is generally recommended. Consulting with a registered dietitian can provide personalized guidance.
- How long does it take to see improvements in PCOD and PCOS symptoms with dietary changes?
- The timeline for seeing improvements in symptoms may vary depending on factors such as the severity of symptoms, adherence to dietary and lifestyle changes, and individual response to treatment. Patience and consistency are key.
- Are there any foods or supplements to avoid?
- While there are no strict rules, individuals with PCOD and PCOS may benefit from limiting processed foods, refined carbohydrates, sugary snacks, and trans fats. It’s essential to consult with a healthcare professional before making significant dietary changes.
- Where can I find more information and support for managing PCOD and PCOS through diet?
- Additional resources, support groups, and healthcare professionals specializing in PCOD and PCOS management can provide further information, guidance, and support tailored to individual needs.